Gari Clifford is an academic who keeps his eyes fixed on real-world problems. His work in machine learning and signal processing is centered on improving some of the world's most burdensome and overlooked healthcare issues.
Clifford, now the tenured chair of the Department of Biomedical Informatics at Emory University and a professor of Biomedical Engineering at Georgia Institute of Technology, got his start in theoretical physics. But near the end of his master’s degree in the mid 90’s, his interests began to change. Conway’s Game of Life spurred him to think about ways to actually measure complex biological systems. Neural networks seemed like the most reasonable answer.
Finding a group working on neural networks in the ‘90s wasn’t easy. But once he made his way to Oxford in 1998, where he pursued a biomedical engineering PhD, Clifford found himself learning and working at the epicenter of British artificial intelligence. He gained steady experience — not just in building neural networks, but also in processing the data properly.
Oxford is also where Clifford “became profoundly interested in solving real-world problems.” At first, his research focused on using machine learning to predict cardiovascular events and critical care needs in hospitals. “That’s where all the data was,” he explains.
Transforming healthcare
After graduate school, Clifford started to get excited about new areas, particularly neuropsychiatry and maternal-fetal health.
“These were the biggest areas where I could have the biggest effect,” Clifford said. “And they’ll have the biggest effect in low- to middle-income countries, which is where I’m most interested in making a difference.”
Edge machine learning is going to transform healthcare.
He’s since held research and faculty positions at MIT, Oxford, and more recently Emory and Georgia Tech, the latter two because he wanted to be more embedded in healthcare systems. He describes his lab as “applying machine learning to whatever problems doctors come up with.” But, he explains, his “secret agenda,” is to see it change healthcare entirely. And for that to happen, edge machine learning — machine learning done in real time and on edge devices — is the key, he said.
“Edge machine learning is going to transform healthcare,” Clifford predicts. Rather than processing data in the cloud, edge machine learning relies on smart devices that use deep machine learning algorithms to process data locally and in real time.
The cloud is still essential to collect the initial data and train the model. Scaling this work requires a large vendor like AWS, Clifford said. Only once the ML model is trained on the cloud can it then be run off the edge sensors in real time. Edge sensors continue to update the model locally, and the data only needs to be pushed to the cloud periodically to prevent model drift and share local updates across all sensors. “The models are much smaller than the data,” Clifford said. “So not only does this reduce the energy and bandwidth needed, but it can preserve the privacy of the patient.”
Monitoring patient environments
Currently, the Clifford Lab — now in its twelfth year and supporting 12 graduate students and six postdoctoral scholars — is using edge machine learning to monitor patient environments. While today’s healthcare system doesn’t ignore a patient’s social support system, such as their interactions with friends, relatives or care providers, it also doesn’t record them, Clifford explained.
A complete picture of an individual’s support system could inform their care, he adds. For instance, decreased interaction with others, changes in their social circle or word choices, and decreased daily travel can all indicate a worsening of the patient’s condition. And they can be easily measured with a smartphone app running edge technology. This strategy is particularly important for the maternal and neuropsychiatry patient populations Clifford is working with, because “traditional healthcare is quite limited for these patient groups,” he said.
In 2018, Clifford received an Amazon Machine Learning Research Award for this work. The funding from Amazon allowed Clifford’s team to develop prototypes and partially funded two PhD students working on the project. They developed audio and Bluetooth algorithms that can run on Raspberry Pis to track who is going in and out of a patient’s hospital care environment. Using the audio and Bluetooth data as a diagnostic tool, the team hopes to understand whether a patient is degenerating quickly and what might be the cause.
“Based on the data, maybe we can come up with interventions — like a sleep intervention — that would reduce deterioration,” Clifford said.
“We started by developing [this technology] for in-hospital use because it allows for rapid development. The hospital is like an experimental environment that's easier to control. It’s much more difficult to do that in someone's home,” he added. But that’s the direction in which his team is moving.
Helping patients stay at home longer
One project Clifford’s group is working on uses the same Raspberry Pis with added sensors to monitor patients with a range of neuropsychiatry issues, including schizophrenia, Alzheimer’s, mild cognitive impairment, Parkinson’s disease, and postpartum depression.
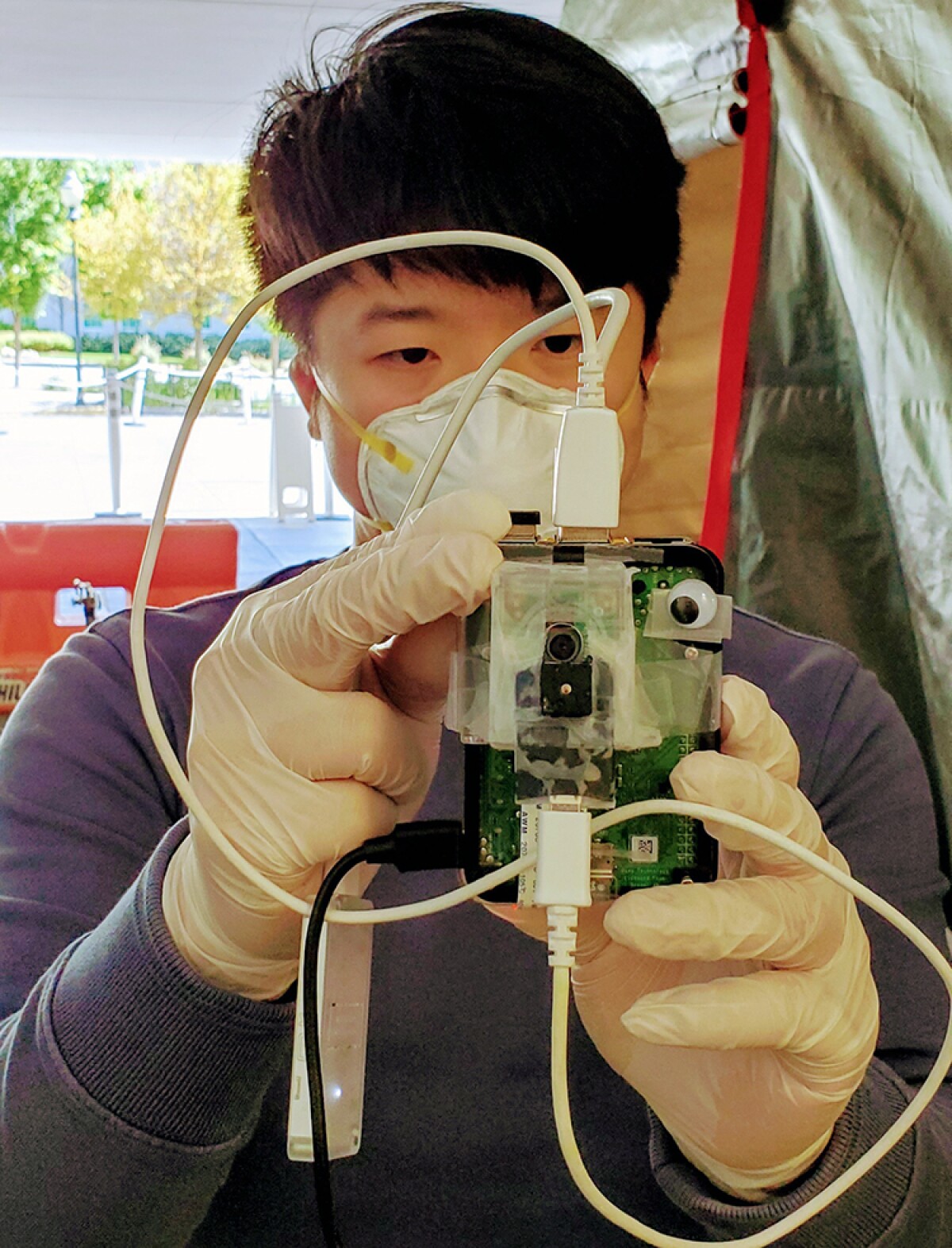
The strategy is to deploy Raspberry Pi devices in these patients’ home environments to monitor their interactions, movement and who comes and goes. Monitoring and managing the patient environment — such as how often they see a healthcare provider, their sleeping patterns, or how often they communicate with others — could help patients live in their homes longer (as opposed to hospitalization) and improve quality of life, Clifford said.
Most importantly for Clifford, the low cost of the tiny Raspberry Pi devices means this strategy is cost-effective. It can be rapidly scaled and deployed in middle- and low-income countries, places where mental and maternal health create an enormous burden but go largely unmanaged.
“It’s an exciting phase,” Clifford said. But many challenges are ahead, like acceptance of the technology. “As we expand sensors and tech, people are obviously concerned about privacy,” he noted. A 2019 study by Pega found that only 30% of respondents felt comfortable with businesses that use artificial intelligence to interact with them.
The importance of developing with inclusivity
As this technology develops, it’s critical to pull underrepresented groups into the process, Clifford explains. Artificial intelligence as an industry tends to be very homogeneous, he notes, and building trust will require that people from different cultures and backgrounds have a hand in its development.
Comfort levels with this technology are not likely to be any higher in the healthcare realm. “There is systemic distrust of this kind of technology, especially in disparity populations,” Clifford said. “And a history of the medical research community exploiting minority populations.”
Clifford’s lab invests significant time trying to build that trust.
In a collaboration with the Morehouse School of Medicine, the team built an app with Amazon Web Services (AWS), leveraging cloud-based computing and infrastructure resources to measure young African Americans’ exposure to different factors that affect cardiovascular disease, such as exercise, healthy food, and air pollution. Community engagement leaders in Atlanta facilitated the data collection, and several interested community members were trained and brought on to the development team. The aim is “to build the infrastructure for them and with them,” Clifford said. The app has just been made open source and “the hope is we have built a substrate the community could build companies out of.”
[The midwives] have fully taken ownership, and they don’t need us anymore. That was the best end result I’ve had with my research, ever.
In Guatemala, a midwife organization Clifford’s group has been collaborating with to predict maternal-fetal health outcomes has completely taken ownership of the technology. The strategy collects inputs like low-cost ultrasound data and pictures of daily blood pressure, and the data, once computed via AWS (Clifford’s team utilized AWS tools like Elastic Cloud Compute, Elastic Load Balancing, Relational Database Service, and GuardDuty, among others) can help predict fetal health.
Next up, Clifford is in search of funding to put that algorithm on the ultrasound device so the computing can be done locally. But in the meantime, the midwives have adopted the technology as the standard of care and reported that they hadn’t lost a single patient in the deployment area over last year.
“They have fully taken ownership, and they don’t need us anymore,” Clifford said. “That was the best end result I’ve had with my research, ever.”


















